Abstract
Chronic pain is a widespread and complex phenomenon, driven by a diverse range of factors. Pain management has become a significant concern over the past several decades in the United States as controversy has grown surrounding the use of opioids for chronic pain management, the use of which has led to abuse and addiction. The Centers for Disease Control and Prevention (CDC) reports that 128 people die in the United States every day from an opioid overdose, whether obtained illicitly or by prescription.2 While opioids remain one of the frontline methods for pain management, their long term safety and efficacy has come under scrutiny. As with any complex systemic issue, there are many contributing factors to chronic pain and pain management. This paper proposes that the experience of awe – specifically elicited by design of the built environment – can serve as an innovative, non-pharmacological pain management tool. Awe is an emotional response to perceptually vast stimuli, precipitating accommodation or a shift in existing mental structures.3 The author hypothesizes that awe can be used as a form of the proven self-regulating pain management method known as reappraisal. Pain reappraisal is cognitive reframing of the context and meaning of pain, changing the value that pain is assigned and resulting in decreased pain perception.4 This paper explores the pertinent intersection of emotions, neuroscience, and the impact of the physical environment on our health and wellbeing. The intention of this paper is to call for a new line of research and does not attempt to address methods or results at this time.
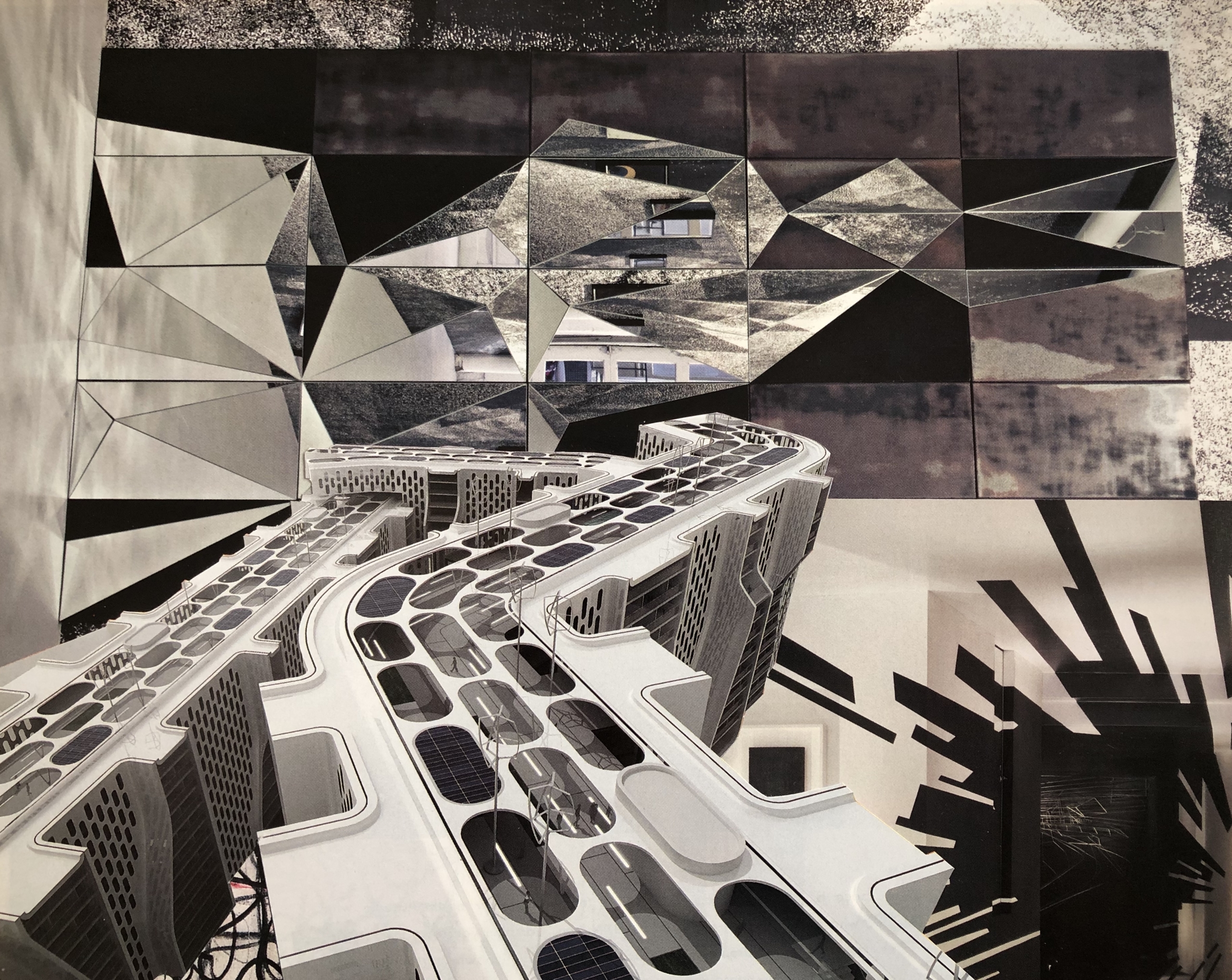
Cover Image: Paper Architecture [Collage]. Provided by the author1
Overview of pain
Chronic pain is characterized by continuously activated pain signals that can be triggered by nociceptive pain (pain from an injury) or neuropathic pain (damage to the peripheral or central nervous system). Chronic pain differs from acute pain in that it can linger long after the initial injury or damage to the body has healed. An important difference between acute and chronic pain is the difference in appraisal.5 Acute pain is often appraised as having an identifiable cause and an expected resolution whereas chronic pain is appraised as pain with no known end that is dissociated from the initial cause.6 Chronification is the process through which acute pain transitions into chronic pain. The processes that contribute to the chronification process are highly individual, informed by genetics, environment, gender, stressors, and socioeconomic status.7
Chronic pain is often associated with comorbidities such as, among others, depression, anxiety, mood alterations, and fatigue. Chronic pain has become a public health crisis in the United States, increasing health costs, and decreasing productivity. In 2016, approximately 20% of U.S. adults had chronic pain (approximately 50 million), and 8% of U.S. adults (approximately 20 million) had high-impact chronic pain.8 This CDC study showed that poverty, education below a high school level, and public health insurance are the strongest indicators in determining populations suffering from chronic pain and associated conditions.
Chronic pain in the individual is influenced by a range of factors, both discrete and systemic. Injury, illness, genetics, personality, and experience are among the factors that influence pain in an individual. Just as influential are systemic factors such as poverty, education, and access to the medical system and health insurance. This confluence of factors leading to chronic pain “has negative consequences to individual persons, their families, and society as a whole”.9 This multidimensional nature of chronic pain means that pain “is not heterogeneous but personalized”, requiring that healthcare providers investigate and understand the individual in pain.10
Since the early 1990s, opioids have become widely prescribed for effective pain management following false reassurances from the pharmaceutical industry of their safety.11 Addiction, abuse, and overdose deaths followed. According to the CDC, even when used properly, opioids have side effects including, among others: physical dependence, tolerance (requiring ever-increasing dosages), increased sensitivity to pain, and depression.12 There are certainly appropriate uses for this class of drugs, but the widespread use and subsequent addiction crisis, paired with little evidence to suggest that opioids are effective long-term, suggests that other methods of pain management must be researched and considered.
There are currently many available pain management strategies that include: medication, surgical intervention, physical therapy, exercise, psychological therapy, cold and/or heat application, and mind-body treatments. According to Marriane Reddan and Tor Wager, there are three strategies of self-regulation for pain control: acceptance, attentional control, and reappraisal. Acceptance is the process of ceasing to resist pain and allow for its existence without judgment, neutralizing the emotional component of pain.13 Attentional control involves directing attention away from pain. In studies examining chronic pain, this strategy has exhibited the enigmatic effect of increasing pain immediately following the experiment.14,15 Pain reappraisal is a type of cognitive reframing of the context and meaning of pain, changing the value pain is assigned.16
Neurophysiology of reappraisal and the introduction of awe as a form of reappraisal
Chronic pain is correlated with long-lasting abnormalities in the brain, associated with decreased gray matter in the regions known to control pain processing and regulation, mood regulation, and cognition.17, 18 Comorbidities such as depression and anxiety are correlated with this decrease in gray matter.19, 20 In MRI cross-sectional brain imaging studies, acute pain, and chronic pain activate different areas of the brain.21 In the process of chronification the brain signature of pain shifts from the nociceptive regions (insula, anterior cingulate cortex, thalamus, and basal ganglia) to the limbic system and emotional circuitry (medial prefrontal cortex, amygdala, and basal ganglia).22 Understanding this shift from the pain regions of the brain to the emotion regions can help inform pain management techniques that target the emotional components of pain such as appraisal, catastrophizing, and fear.
Cognitive reappraisal acts upon the regions of the brain associated with processing affective meaning, commonly in the form of Cognitive Behavioral Therapy (CBT). Wager et al,23 found two pathways that correlated with cognitive reappraisal. The pathway between the ventrolateral prefrontal cortex and the amygdala predicted the failure of cognitive reappraisal while the pathway between the ventrolateral prefrontal cortex and the nucleus accumbens predicted successful cognitive reappraisal. The ventrolateral prefrontal cortex is part of the cerebral network dedicated to attention. It has been hypothesized that the ventrolateral prefrontal cortex governs reflexive reorienting.24 This important mechanism allows the brain to shift attention, making it possible to switch tasks and enabling us to reorient our attention to events occurring outside our current focus of attention. Cognitive reappraisal in the form of CBT has proven successful in pain management through modification of the understanding, expectations, and beliefs related to pain.25
This paper proposes the consideration of awe as a form of self-regulating pain management, akin to cognitive reappraisal. Reappraisal and awe have similar characteristics, primarily the ability to shift perspective, through updating existing mental structures. If the experience of awe can shift perspectives similarly to cognitive reappraisal then awe should be considered as an innovative pain management tool.
Characteristics and impacts of awe
Awe is defined as “an emotional response to perceptually vast stimuli that overwhelm current mental structures, yet facilitate attempts at accommodation”.26 Awe has only recently come under the scrutiny of researchers studying emotion.27 Awe is known to cause a range of feelings and behaviors such as altered time perception28, ego transcendence and generosity29, self-diminishment and increased orientation towards the collective30, interconnectedness31, 32, feelings of uncertainty and a sense that dichotomies can be transcended or resolved.33, 34
The two primary components contributing to the state of awe are “vastness” and “accommodation”.35 The perceptual response of vastness is defined as anything experienced as larger than the self and can encompass physical space, time, the complexity of detail, ability, conceptual vastness, or volume of human experience.36 The ensuing cognitive response of accommodation refers to the neurophysiological process of updating existing mental architecture when the current schema fails to make sense of a vast experience.
Researchers are beginning to understand what function awe serves in the human experience. Awe is thought to play an important role in the diminishment of self and subsequent advancement of the social collective.37 Michelle Shiota offers the theory that awe may play an important role in knowledge formation.38 In research studies, awe appears to improve awareness and understanding of the surrounding environment which is likely the consequence of the process of accommodation. In addition to its role in knowledge formation, research has begun to link awe to good health and wellbeing.39, 40, 41
Awe in the built environment
The emotion of awe is most commonly associated with vast experiences in nature. Music, architecture, art, complex mathematical concepts, interpersonal connection, and remarkable human achievements are other elicitors of the emotion of awe. Throughout history, architects and builders have designed and constructed architecture to elicit specific responses from its inhabitants or visitors. Whether it was the great pyramids of ancient Egypt, the soaring light-filled cathedrals of Europe, or the ordered architecture of the Third Reich, architects have purposefully manipulated buildings to express messages respectively of power, faith, and fear. A recent study42 showed that monumental architecture causes people to exhibit behavioral freezing, a component of awe. In 2019, architecture student Wendi Yan explored possible design features that contribute to a sense of awe, including repetition and magnitude which provide a sense of infinity, silence or places of pause, the introduction of a safety threat similar to prospect and refuge, and references to nature represented through biophilic forms or natural materials.43 Architecture is an embodied and emotional experience with the ability to shift human behavior and elicit emotional responses such as awe. The architectural researcher, Julio Bermudez has introduced rigorous scientific research that examines the embodied and emotional response that architecture elicits, bridging the gap between science and phenomenology.44 This paper hypothesizes that intentionally introducing awe into the built environment will contribute to reframing and reduction of the perception of chronic pain.
Building on the research of Wendi Yan, awe can be introduced into healthcare environments in multiple ways with the intention of disrupting pain perception. The concept of infinity is one of boundlessness, which stands in direct contradiction to the human condition. Infinity can be expressed in the built environment through repeating forms that suggest endlessness and spaces that communicate magnitude. This juxtaposition of being bound by the limitations of a body in pain with the concept of infinity can bring a moment of awareness, similar to behavioral freezing, allowing a person in pain to step outside of their current experience. This creates a moment of pause, an opportunity to consider the meaning of pain and potentially reappraise its significance and value. Physical moments of pause in the environment are also places for similar opportunities, places that allow a person to engage their condition, instead of merely seeking distraction from it. These places of pause can be articulated in many possible ways such as an alcove within a path of travel, a window seat for reflection, or a bench nestled in a garden. In addition to facilitating pause, these spaces provide an opportunity for what Yan refers to as ‘safe threat’, a place to safely observe one’s surroundings. The essence of nature as a foundational elicitor of awe is its ability to trigger connectedness.45,46 In a similar manner to infinity, nature creates awareness of our human experience within a greater context. Cognitive reappraisal and the emotion of awe both shift our perspective outside of our current experience. Architectural spaces that deliberately incorporate moments of awe, through the application of these design principles, present the potential to disrupt pain perception.
There are many healthcare settings that could benefit from the impact of an intentionally designed environment that facilitated a reduction in the experience of pain. These include waiting rooms in hospitals and clinical settings, rehabilitation centers, addiction treatment facilities, oncology treatment centers, labor and delivery units, and hospice care facilities. The design and phenomenon of architecture functions centrally in our embodied and emotional experience of the world.
Future research into the effects of the built environment on pain
Since the seminal work of Roger Ulrich47, there has been growing interest in the impact of the built environment on pain and wellbeing. Ulrich’s study explored the restorative influences of a window with a view of nature in recovering cholecystectomy patients. Subsequent studies have examined the effects of light, nature, and virtual reality as environmental factors impacting pain control.48 These environmental factors utilize different neural processes from awe and reappraisal, opening a new avenue for future research to examine the effect of the environment on pain and study the impact of awe and its similarity to reappraisal, which is a known tool for self-regulating pain control. Future research should examine the mechanism for awe interrupting the pain cycle, examining whether awe helps decrease rumination or increases motivational and problem-solving strategies. There is immense potential in exploring the positive benefits that architecture can have with regards to pain management.
References
1 Hoffman, M. (2014). Paper Architecture [Collage]. Provided by the author.
2 Centers for Disease Control and Prevention. (2020, March 19). Understanding the Epidemic. Retrieved from https://www.cdc.gov/drugoverdose/epidemic/index.html
3 Keltner, D. & Haidt, J. (2003) Approaching awe, a moral, spiritual, and aesthetic emotion, Cognition and Emotion, 17:2, 297-314, DOI: 10.1080/02699930302297
4 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
5 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
6 Ibid.
7 Borsook, D., Youssef, A. M., Simons, L., Elman, I., & Eccleston, C. (2018). When pain gets stuck: the evolution of pain chronification and treatment resistance. Pain, 159(12), 2421.
8 Dahlhamer J, Lucas J, Zelaya, C, et al. (2016) Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults — United States. MMWR Morb Mortal Wkly Rep 2018;67:1001–1006. DOI: http://dx.doi.org/10.15585/mmwr.mm6736a2external icon.
9 Ibid.
10 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
11 US Dept of Health and Human Services. (2019, September 4). What is the U.S. Opioid epidemic? Retrieved from https://www.hhs.gov/opioids/about-the-epidemic/index.html
12 Centers for Disease Control and Prevention. (2017, August 29). Prescription Opioids. Retrieved from https://www.cdc.gov/drugoverdose/opioids/prescribed.html
13 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
14 Goubert, L., Crombez, G., Eccleston, C., & Devulder, J. (2004). Distraction from chronic pain during a pain-inducing activity is associated with greater post-activity pain. Pain, 110(1-2), 220-227.
15 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
16 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
17 Bushnell, M. C., Case, L. K., Ceko, M., Cotton, V. A., Gracely, J. L., Low, L. A., … & Villemure, C. (2015). Effect of environment on the long-term consequences of chronic pain. Pain, 156(0 1), S42.
18 Davis KD, Moayedi M. (2013). Central mechanisms of pain revealed through functional and structural MRI. J Neuroimmune Pharmacol, 8(3):518-534. doi:10.1007/s11481-012-9386-8
19 Bushnell, M. C., Case, L. K., Ceko, M., Cotton, V. A., Gracely, J. L., Low, L. A., … & Villemure, C. (2015). Effect of environment on the long-term consequences of chronic pain. Pain, 156(0 1), S42.
20 Gustin, S. M., Peck, C. C., Wilcox, S. L., Nash, P. G., Murray, G. M., & Henderson, L. A. (2011). Different pain, different brain: thalamic anatomy in neuropathic and non-neuropathic chronic pain syndromes. Journal of Neuroscience, 31(16), 5956-5964.
21 Hashmi, J. A., Baliki, M. N., Huang, L., Baria, A. T., Torbey, S., Hermann, K. M., … & Apkarian, A. V. (2013). Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain, 136(9), 2751-2768.
22 Ibid.
23 Wager, T. D., Davidson, M. L., Hughes, B. L., Lindquist, M. A., & Ochsner, K. N. (2008). Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron, 59(6), 1037-1050.
24 Corbetta, M., Patel, G., & Shulman, G. L. (2008). The Reorienting System of the Human Brain: From Environment to Theory of Mind. Neuron, 58(3), 306–324.
25 Reddan, M. C., & Wager, T. D. (2019). Brain systems at the intersection of chronic pain and self-regulation. Neuroscience Letters, 702, 24-33.
26 Shiota, M. N., Keltner, D., & Mossman, A. (2007). The nature of awe: Elicitors, appraisals, and effects on self-concept. Cognition and emotion, 21(5), 944-963.
27 Keltner, D. & Haidt, J. (2003) Approaching awe, a moral, spiritual, and aesthetic emotion, Cognition and Emotion, 17:2, 297-314, DOI: 10.1080/02699930302297
28 Rudd, M., Vohs, K. D., & Aaker, J. (2012). Awe Expands People’s Perception of Time, Alters Decision Making, and Enhances Well-Being. Psychological Science, 23(10), 1130–1136.
29 Piff, P. K., Dietze, P., Feinberg, M., Stancato, D. M., & Keltner, D. (2015). Awe, the small self, and prosocial behavior. Journal of personality and social psychology, 108(6), 883.
30 Bai, Y., Maruskin, L. A., Chen, S., Gordon, A. M., Stellar, J. E., McNeil, G. D., Peng, K., Keltner, D. (2017). Awe, the diminished self, and collective engagement: Universals and cultural variations in the small self. Journal of Personality and Social Psychology, 113(2), 185-209
31 Shiota, M. N., Keltner, D., & Mossman, A. (2007). The nature of awe: Elicitors, appraisals, and effects on self-concept. Cognition and emotion, 21(5), 944-963.
32 Yang, Y., Hu, J., Jing, F., & Nguyen, B. (2018). From Awe to Ecological Behavior: The Mediating Role of Connectedness to Nature. Sustainability, 10(7), 2477.
33 Maslow, A.H. (1964). Religions, values, and peak experiences. London: Penguin Books Limited.
34 Keltner, D. & Haidt, J. (2003) Approaching awe, a moral, spiritual, and aesthetic emotion, Cognition and Emotion, 17:2, 297-314, DOI: 10.1080/02699930302297
35 Keltner, D. & Haidt, J. (2003) Approaching awe, a moral, spiritual, and aesthetic emotion, Cognition and Emotion, 17:2, 297-314, DOI: 10.1080/02699930302297
36 Shiota, M. N., Keltner, D., & Mossman, A. (2007). The nature of awe: Elicitors, appraisals, and effects on self-concept. Cognition and emotion, 21(5), 944-963.
37 Bai, Y., Maruskin, L. A., Chen, S., Gordon, A. M., Stellar, J. E., McNeil, G. D., Peng, K., Keltner, D. (2017). Awe, the diminished self, and collective engagement: Universals and cultural variations in the small self. Journal of Personality and Social Psychology, 113(2), 185-209.
38 Shiota, M. N., Keltner, D., & Mossman, A. (2007). The nature of awe: Elicitors, appraisals, and effects on self-concept. Cognition and emotion, 21(5), 944-963.
39 Anderson, C. L., Monroy, M., & Keltner, D. (2018). Awe in nature heals: Evidence from military veterans, at-risk youth, and college students. Emotion, 18(8), 1195.
40 Gordon, A. M., Stellar, J. E., Anderson, C. L., McNeil, G. D., Loew, D., & Keltner, D. (2017). The dark side of the sublime: Distinguishing a threat-based variant of awe. Journal of personality and social psychology, 113(2), 310.
41 Stellar, J. E., John-Henderson, N., Anderson, C. L., Gordon, A. M., McNeil, G. D., & Keltner, D. (2015). Positive affect and markers of inflammation: Discrete positive emotions predict lower levels of inflammatory cytokines. Emotion, 15(2), 129-133.
42 Joye, Y., & Dewitte, S. (2016). Up speeds you down. Awe-evoking monumental buildings trigger behavioral and perceived freezing. Journal of Environmental Psychology, 47, 112–125. https://doi.org/10.1016/j.jenvp.2016.05.001
43 Yan, W. (2019). Neuroscience informs design, now what? Towards an awe-inspiring spatial design. London: Conscious Cities Anthology 2019: Science-Informed Architecture and Urbanism. ISSN 2514-6815 DOI:10.33797/CCA19.01.19
44 Bermudez, J. (2011). Empirical aesthetics: the body and emotion in extraordinary architectural experiences. Proceedings of the 2011 Architectural Research Centers Consortium:“Considering Research, 369-380.
45 Shiota, M. N., Keltner, D., & Mossman, A. (2007). The nature of awe: Elicitors, appraisals, and effects on self-concept. Cognition and emotion, 21(5), 944-963.
46 Yang, Y., Hu, J., Jing, F., & Nguyen, B. (2018). From Awe to Ecological Behavior: The Mediating Role of Connectedness to Nature. Sustainability, 10(7), 2477.
47 Ulrich, R. S. (1984). View through a window may influence recovery from surgery. science, 224(4647), 420-421.
48 Malenbaum, S., Keefe, F. J., Williams, A., Ulrich, R., & Somers, T. J. (2008). Pain in its environmental context: implications for designing environments to enhance pain control. Pain, 134(3), 241.